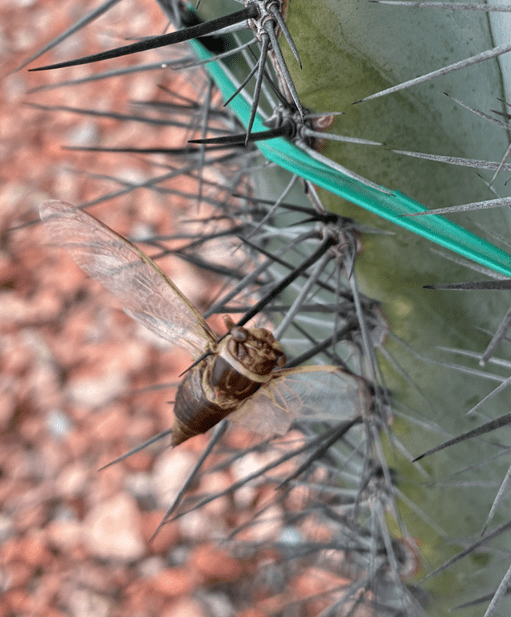
Catch of The Day at Phoenix City Grill
My Experience with a Gastronomy Feeding Tube
For seven or eight months, I relied on a gastronomy feeding tube. While I cannot recall the exact date it was installed—nor have I been able to locate any records—I remember very clearly when it was removed. Before sharing more details about my specific experience, it is useful to describe feeding tubes in general, and mine in particular.
Types of Feeding Tubes
There are four main types of feeding tubes. My tube, known as a gastronomy tube (G-tube), connects directly to the stomach through an opening cut in the abdomen at the time of installation. Admittedly, the procedure is not pleasant. However, having a hole in the abdomen and stomach seems less troublesome than the alternative types that reach the stomach or small intestine by passing a tube through the nose or mouth and down the esophagus.
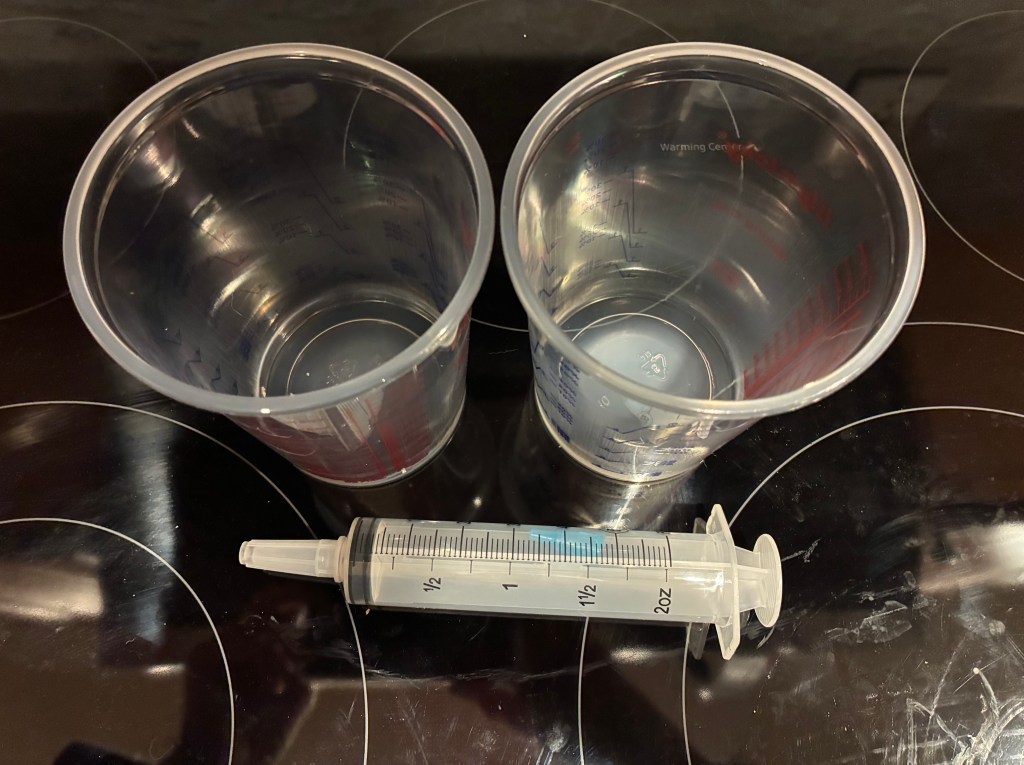
Additionally, there is the jejunostomy tube (J-tube), which bypasses the stomach and connects directly to the small intestine through a surgically created opening. With all these tubes, nutrients are delivered in liquid form and inserted either with a syringe or a drip mechanism.
Why I Needed a Feeding Tube
My feeding tube was installed because cancer treatment dramatically affected my sense of taste. Chemotherapy impacts the taste buds via the salivary glands, while radiation affects both the taste buds directly and the nerves in the treatment area. Since my cancer was esophageal, I suspect radiation was responsible for most of the changes I experienced in taste. This is supported by the fact that, for me, everything tasted like cardboard or had no taste at all. Chemotherapy tends to make food taste metallic. Unfortunately, the effects of chemotherapy last for weeks, but radiation’s impact can persist for months—or may never be fully resolved. It has now been eight months since my treatment ended, and I am still struggling with some food.
Feeding Methods: Drip vs. Syringe
At first, my caregivers (in the hospital and rehab) preferred to use a drip mechanism for feeding. I am not sure why they wanted the drip vs a syringe, but using the drip always took longer than an hour, and sometimes even more. The extended feeding times were frustrating because I had to remain attached to a nutrient bag, which needed to be positioned above my stomach, resulting in limited mobility. While still in rehab, I switched to the syringe method, which was much quicker and more convenient.
The end of the tube
In December (2025) I had the tube replaced. I went home from the procedure and tested it (by using the Nestle Nutren (1.5 g protein per 250 ml). That was the last time it was used. That was difficult to do because I had to make up the calories and protein that the Nutren was supplying. I had already been supplementing the Nutren with some food (like ice cream, candy and protein drinks -that I detested). To my surprise, the calories were easier than the protein.
Finally on January 9 (2026) I had the tube removed. A week later I celebrated at Phoenix City Grill with the catch of the Day which is pictured above. I still track calories and protein – AI is great for that task. Along the way I was surprised by my reactions to several foods. The first two foods I noticed that tasted as I remembered were frozen strawberries (as in Dairy Queen sundaes) and root beer (as in Shake Shack root beer floats). Fish is almost always good whereas beef and pork not so much. One last comment, beer is better than wine. For a snob like me, that is very surprising.

Just removed!